Dispelling depression myths
- Category: General, Mental Health
- Posted On:
- Written By: Boulder Community Health

October is National Depression & Mental Health Screening Month
Five percent of the global adult population experiences depression, which involves a persistent depressed mood, sadness, or loss of pleasure or interest in activities for long periods of time. Depression is different from regular mood changes and feelings about everyday life. It can affect all aspects of life, including relationships with family, friends and community. It can also result from or lead to problems at school and work.
During a depressive episode, a person experiences a depressed mood (feeling sad, irritable, empty). Other symptoms may include poor concentration, feelings of excessive guilt or low self-worth, hopelessness about the future, thoughts about dying or suicide, disrupted sleep, changes in appetite or weight, and more.
Depression can affect anyone, especially individuals who have lived through abuse, severe losses or other stressful events. Women are also more likely to experience depression than men, particularly those who are pregnant or have just given birth. Seasonal affective disorder, or SAD, is a type of depression that is characterized by its recurrent season pattern, with symptoms lasting about four to five months per year.
While depression is a common condition, there are still many myths surrounding the disease. This results in a stigma that can harm well-being and can have long-lasting effects.
Here are some of the common myths that everyone can dispel to improve the lives of those who face this illness.
Myth 1: “People with depression aren’t normal.”
Approximately 280 million people in the world have depression. They often struggle, silently. You can be part of the solution for improving the way our community views or talks about mental illness. Depression does not discriminate, and it affects people in different ways. Destigmatizing mental illness is a wonderful step in bringing hope to people.
The National Alliance on Mental Health (NAMI) has some tips on challenging misconceptions; see the person, not the condition; offer support if you think someone is having trouble; and avoid labels such as – challenged, crazy, wacko, normal/not normal, lunatic, psycho/psychopath, special or sufferer.
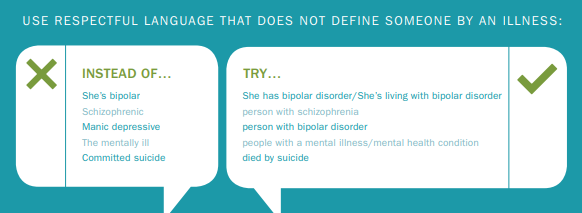
Photo credit: NAMI
Myth 2: “Depression is only triggered after a sad or traumatic event.”
Depression is not always caused by one event or trigger. It’s not a situational disorder; it’s a clinical and chronic illness, meaning it’s much more than a mood or feeling.
Researchers believe several factors can contribute to depression. Trauma, genetics, life circumstances, brain changes, other medical conditions, and drug and alcohol misuse are just a few.
About 21 million U.S. adults—8.4% of the population—had at least one major depressive episode in 2020.
Myth 3: “Antidepressants and counseling work for everyone.”
Treatment is not one size fits all. Depression is usually treated with medication, psychotherapy or a combination of the two. Up to a third of patients with depression, though, don’t respond to those traditional forms of treatment.
Through the Center for Interventional Psychiatry, BCH is proud to offer safe brain therapies, such as electroconvulsive therapy (ECT), as well as newer treatment therapies like transcranial magnetic stimulation (TMS) and ketamine infusion. BCH's highly skilled psychiatrists treat adults with treatment-resistant depression, bipolar disorder and schizophrenia and are dedicated to life-changing health care for chronic, complex mental illnesses.
Mental Health Treatment at BCH
If you are experiencing symptoms of depression yourself, know you are not alone. Be an advocate for yourself and talk with your doctor, lean on your support system and keep an open mind when it comes to your treatment.
Within BCH’s “Behavioral Health Home,” our community members can find appropriate and meaningful care for depression and mental health conditions ranging from simple, to complex, to chronic.
- Behavioral Health Specialists in Primary Care: During a primary care clinic visit, your provider will screen for depression by asking some questions off the PHQ-9 questionnaire. At this time, patients can also address any health concerns about mental health issues: history, symptom quality, or possible shared decision-making around treatment options. If needed, your provider can introduce you to a behavioral health specialist, who are embedded in each of our primary care clinics, with a warm hand off for ongoing care.
- Outpatient Behavioral Health: Addresses a wide range of mental health issues, including anxiety, trauma, depression and attention deficit disorder. We also offer therapy, counseling and online classes.
- Center for Interventional Psychiatry (CIP): Advanced treatment options – including Electroconvulsive Therapy (ECT), Transcranial Magnetic Stimulation (TMS) and ketamine infusions - for mental health disorders, including depression, bipolar disorder, obsessive-compulsive disorder, manic illnesses or schizophrenia.
- Inpatient Behavioral Health: The thoughtfully designed healing environment on the third floor of the Della Cava Medical Pavilion offers intervention, safety and stabilization for adults in acute emotional crisis.
- Emergency Department (ED): Psychiatric evaluations are available 24/7 for community members who don’t feel safe or are in crisis. Mental health holds – or involuntary holds – are also provided if needed.